Intraoperative Neurophysiological Monitoring (IONM) Role in Tibial and Fibular Osteotomy in Pediatric Surgeries
By Admin | July 30, 2020
Faisal R. Jahangiri, MD, CNIM, D.ABNM, FASNM, FASET
Axis Neuromonitoring LLC, Richardson, TX, USA.
Introduction
Intraoperative Neurophysiological Monitoring (IONM) is not used routinely during tibial and fibular osteotomy procedures. Pediatric patients who present with Tibia Vara (Blount's disease), juvenile osteochondrosis, and Genu Valgum (Knock-Knees), etc. are surgically treated with tibial and fibular osteotomy. These patients have a high risk of postoperative weakness or foot drop with or without sensory deficits. The incidence of postoperative neurological deficits ranges from 2% to 20%. The postoperative neurological complications can be minimized by utilizing IONM
- Tibia Vara (Blount's Disease)
- It is a growth disorder of the Tibia (shin bone) that causes the lower leg to angle inward, resembling a bowleg.
- Juvenile Osteochondrosis
- Occur in children characterized by interruption of the blood supply of a bone, in particular to the epiphysis, followed by localized bony necrosis and later, re-growth of the bone.
- Genu Valgum:
- Commonly called "knock-knees" is a condition where the knees angle in and touch one another when the legs are straightened.
Patient History
A 4-year-old female patient presented with an Infantile Blount's disease of the left leg admitted for the left leg proximal tibial and fibular osteotomy. Concerns during Tibial and Fibular osteotomies included ipsilateral lower limb motor and sensory function, due to peroneal nerve injuries by osteotomy at the fibular neck. Total Intravenous Anesthesia (TIVA) without any muscle relaxant, inhalational agent, or dexmedetomidine was planned.
Figure 1: A multimodality monitoring approach during tibial and fibular osteotomy procedures.
Method
A multimodality IONM approach included Somatosensory Evoked Potentials (SSEPs-Peroneal and Posterior Tibial nerves), Transcranial electrical Motor Evoked Potentials (TCeMEPs), spontaneous Electromyography (s-EMG) and triggered Electromyography (t-EMG). Both SSEP and TCeMEP were utilized for monitoring the sensory and motor nerve fibers. S-EMG for detecting any nerve root irritation and t-EMG to help the surgeon in localizing the nerves.
By using both posterior tibial and peroneal nerve SSEP stimulation (at the ankle) with lower limb TCeMEP recordings more precise status of sensory and motor pathways was possible during the surgical correction. Similarly, s-EMG and t-EMG was performed to localize nerve irritation more accurately


Figure 2. Intraoperative image of the left leg of a patient with skin prepped and draped for surgery -recording and stimulation electrodes placed for SSEP, EMG, and TCeMEP. The intraoperative X-ray shows a rod placed after the osteotomy procedure.
Results
During the surgical procedure, there was a sudden loss of left peroneal SSEP and TCeMEP. The technologist immediately informed the surgeon about the changes. Surgical interventions consisting of additional fibular resection was made. The sensory and motor data changes were due to the peroneal nerve entrapment at the osteotomy site. After the appropriate surgical intervention, neurophysiological signals returned to the baseline. Triggered EMG was performed to identify any nerve at the surgical site. Postoperatively, the patients presented with no neurologic deficit.
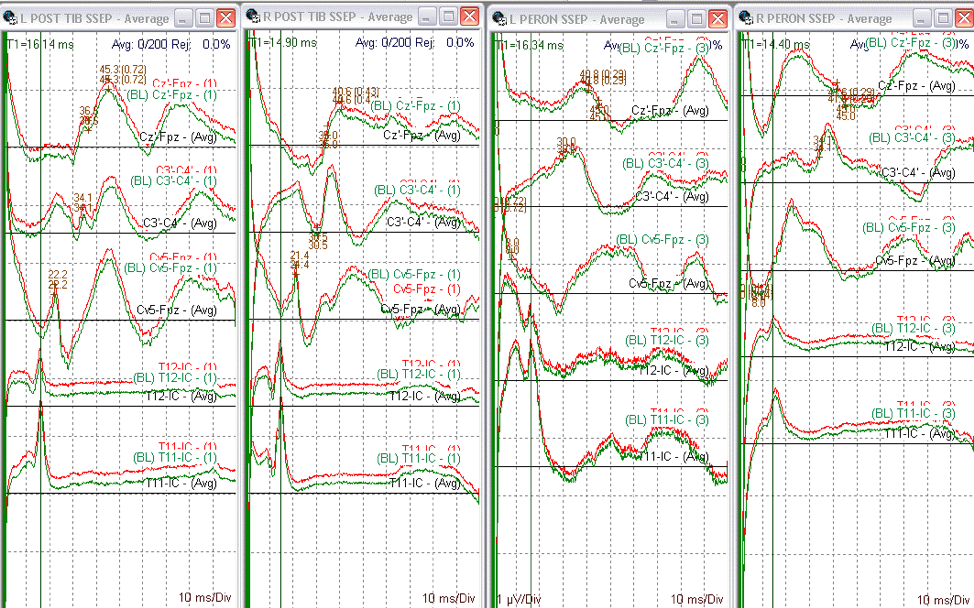
Figure 3: Somatosensory evoked potentials (SSEP) data from posterior tibial and left peroneal nerve bilaterally. Lumbar potential (LP) responses also present with good morphology.
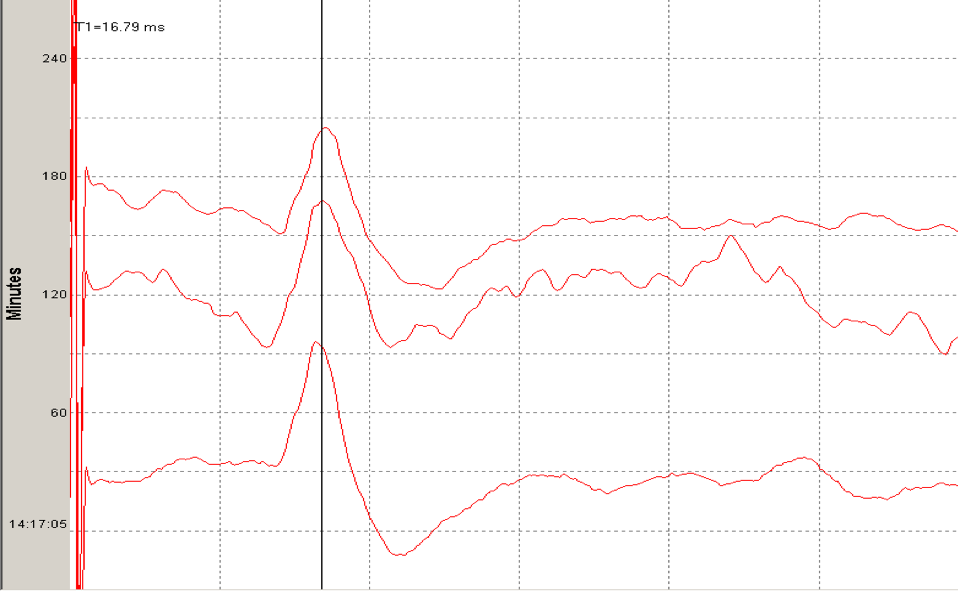
Figure 4. Lumbar potential (LP) recording in Somatosensory evoked potentials (SSEP) data. Recording electrodes were placed subdermally at T12, and L1 spinous process referenced to the contralateral iliac crest (IC).
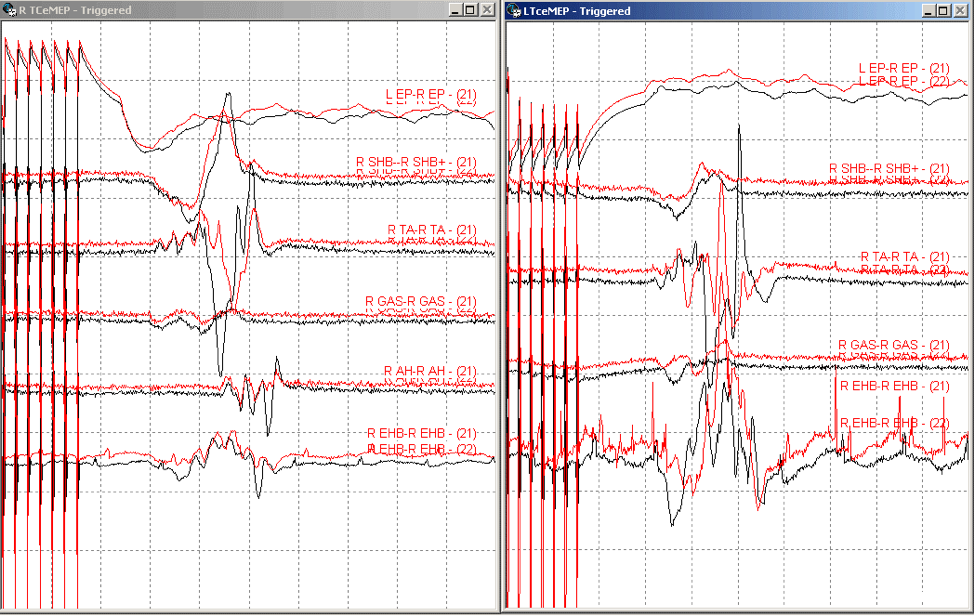
Figure 5. Ipsilateral Transcranial electrical motor evoked potential (TCeMEP) responses from the lower limb muscles. Subdermal needle electrodes placed in biceps femoris short head (SHB), tibialis anterior (TA), gastrocnemius (GAS), abductor hallucis (AH) and extensor hallucis brevis (EHB) muscles.

Figure. 6. Ipsilateral spontaneous EMG (s-EMG) during the osteotomy correction. Subdermal needle electrodes placed in tibialis anterior (TA), peroneus longus (PL), gastrocnemius (GAS), abductor hallucis (AH), and extensor hallucis brevis (EHB) muscles.
Discussion
Utilizing the multimodality IONM with SSEP, TCeMEP, s-EMG, and t-EMG during peripheral nerve surgeries can be highly beneficial to the patient and as well as the surgeon. Besides, by using multimodality IONM, we were able to perform monitoring with a high level of confidence throughout the surgery. Real-time feedback to the surgeon about the nerves can help the surgeon to make the best decision, which may alter the course of treatment. IONM can also minimize any postoperative neurological deficits involving the motor and sensory functions.
Conclusion
In this patient, a multimodality IONM was effectively used for the evaluation of the neural function. The neurophysiological monitoring utilizing SSEP with LP, TCeMEP, and EMG helped in directing the surgeon intra-operatively. During surgeries that put the peripheral nerves at risk of injury, continuous monitoring of the function is desirable. A CNIM certified technologist and a D.ABNM board-certified neurophysiologist performed IONM. A board-certified neurologist with a specialty in IONM was also present online for remote monitoring during the entire surgical procedure.
References:
[1] Jahangiri FR. Multimodality neurophysiological monitoring during tibial/fibular osteotomies for preventing peripheral nerve injuries. Neurodiagn J. 2013;53(2):153?168.
[2] Jahangiri FR, Wimberly R. Multimodality neurophysiological monitoring in tibial/fibular osteotomies for preventing peripheral nerve injuries. Abstracts published in proceedings of Saudi Physical Therapy Conference; May 2012; Riyadh, Saudi Arabia; page 34.
[2] Happel L.T., Kline D.G. (2017) Surgery in the Peripheral Nervous System. In: Koht A., Sloan T., Toleikis J. (eds) Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals. Springer, Cham.
[3] Happel L, Kline D. Intraoperative neurophysiology of the peripheral nervous system. In: Deletis V, Shils J, editors. Neurophysiology in neurosurgery. New York: Academic; 2002. p. 169–94.
[4] Jahangiri FR, Blaylock J, Qadir N, Ramsey JA. Multimodality Intraoperative Neurophysiological Monitoring (IONM) During Shoulder Surgeries. Neurodiagn J. 2020;1?17. doi:10.1080/21646821.2020.1743952.
[5] Jahangiri, FR. Surgical Neurophysiology: An Introduction to Intraoperative Neurophysiological Monitoring (IONM). Second Edition. April 2012.
[6] ABRET Neurodiagnostic Credentialing and Accreditation. (2019, Sep 9). ABRET. Retrieved Sep 9, 2019, from ABRET: https://www.abret.org/candidates/credentials/cnim/
[7] ABNM: American Board of Neurophysiologic Monitoring. (2019, Sep 9). ABNM: American Board of Neurophysiologic Monitoring. Retrieved Sep 9, 2019, from ABNM: American Board of Neurophysiologic Monitoring: http://www.abnm.info/
[10] Gertsch JH, Moreira JJ, Lee GR, Hastings JD, Ritzl E, Eccher MA, Cohen BA, Shils JL, McCaffrey MT, Balzer GK, Balzer JR, Boucharel W, Guo L, Hanson LL, Hemmer LB, Jahangiri FR, Mendez Vigil JA, Vogel RW, Wierzbowski LR, Wilent WB, Zuccaro JS, Yingling CD; membership of the ASNM. (2019). Practice guidelines for the supervising professional: intraoperative neurophysiological monitoring. J Clin Monit Comput, 33(2), 175-183. doi:10.1007/s10877-018-0201-9



