Intraoperative Neurophysiological Monitoring (IONM) During Peripheral Nerve Hand Surgeries
By Admin | June 03, 2020
Intraoperative Neurophysiological Monitoring (IONM) During Peripheral Nerve Hand Surgeries
Faisal R. Jahangiri, M.D., CNIM, D.ABNM, FASNM, FASET 1 ; Tyler C. Mahan, CNIM 1
1 Axis Neuromonitoring LLC, Richardson, TX, USA.
Objective:
This case report illustrates the benefit of utilizing Intraoperative Neurophysiological Monitoring (IONM) during the peripheral nerve surgeries involving the hand. A multimodality IONM approach included Somatosensory Evoked Potentials (SSEP), Dermatomal Sensory Evoked Potentials (DSEP), Electromyography (EMG), Transcranial electrical Motor Evoked Potentials (TCeMEP), Train of Four (TOF).
Case Report:
A 34-year-old male patient presented with a crushing injury of the right hand. The patient had a compartment syndrome of the right side after his injury two years ago. The patient had previous surgeries done for carpal tunnel and proximal forearm release - the patient presented with no sensations in the right palm, index, and middle fingers. The patient had some motor function in his fingers. The surgeon planned to identify the motor and sensory branches of the median nerve, sacrifice the sensory fibers for nerve graft. The anesthetic regimen included less than 0.5 MAC of Sevoflurane with no muscle relaxation after the intubation.
After patient intubation, we placed surface adhesive electrodes for left median SSEP stimulation as a control. The right median nerve was in the surgical field. Therefore, we decided to do Dermatomal Sensory Evoked Potentials (DSEP) by placing the surface adhesive electrodes on the right index finger. The surgeon placed 7.0 mm subdermal needle electrodes in the sterile field for EMG and TCeMEP recordings from the first lumbrical, opponens pollicis, abductor pollicis brevis, flexor pollicis brevis, and abductor digitiminimi muscles.
The baseline SSEP was present in the left hand but absent on the right side. TCeMEP responses were present in the left hand but absent on the right side at the baseline. We used triggered electromyography (t-EMG) to identify the individual branches of the right median nerve by the surgeon. T-EMG responses were observed at 0.5 mA by direct monopolar nerve stimulation. The surgeon received real-time feedback.
After the exposure and 90 minutes into the procedure, we were unable to record t-EMG in the right hand. We increased the stimulation to 4.0 mA but did not record any responses. During the troubleshooting steps, the surgeon was consulted and recommended to remove the tourniquet from the right arm. We were able to produce the t-EMG response fifteen minutes after removing the tourniquet at the baseline 0.5 mA threshold. We were also able to record TCeMEP from all the muscles
in the right hand.
During the neurolysis process right DSEPs from the index finger became reproducible and recordable. The surgeon was immediately notified about the presence of DSEP. The amplitude was smaller, and latency was longer compared to the left hand's SSEP responses. The sensory and motor signals improved during the procedure. The surgeon decided not to resect the damaged sensory branch or perform the nerve graft in the presence of improved somatosensory responses. The signal remained stable until the end of the surgery.
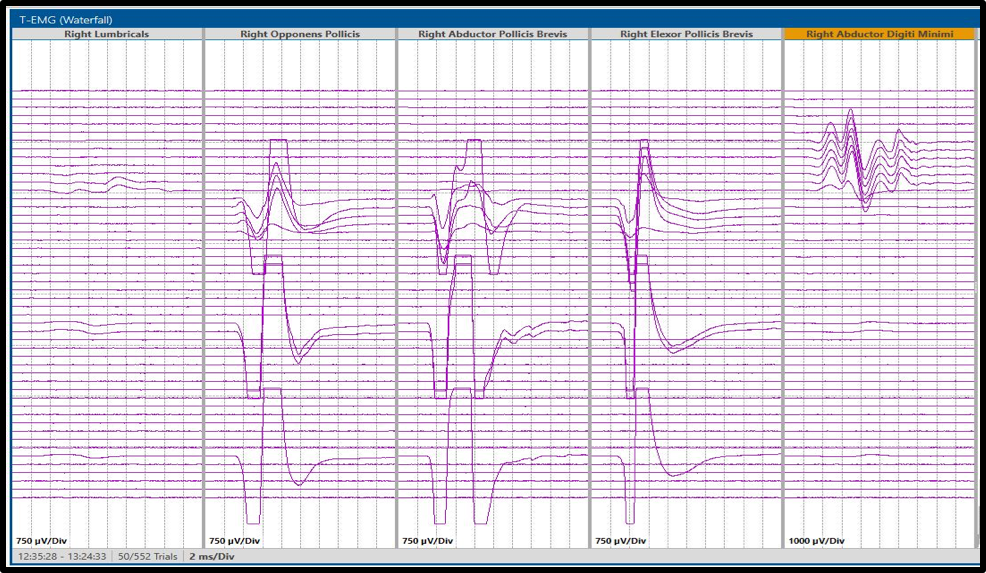
Figure 1: Triggered Electromyogram (t-EMG) responses from hand muscles supplied by the median nerve (Green arrows) and ulnar nerve (Blue arrow).
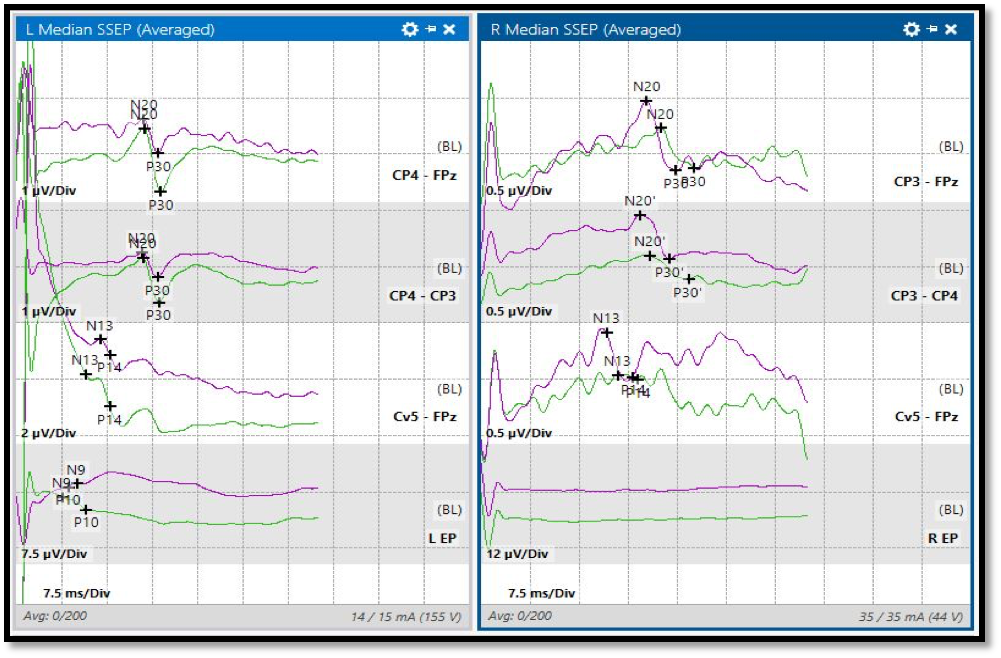 Figure 2: Left Median Nerve SSEP and Right C6 Dermatomal SSEP (Median nerve). Baseline responses (Green) and the final trace (Purple).
Figure 2: Left Median Nerve SSEP and Right C6 Dermatomal SSEP (Median nerve). Baseline responses (Green) and the final trace (Purple).
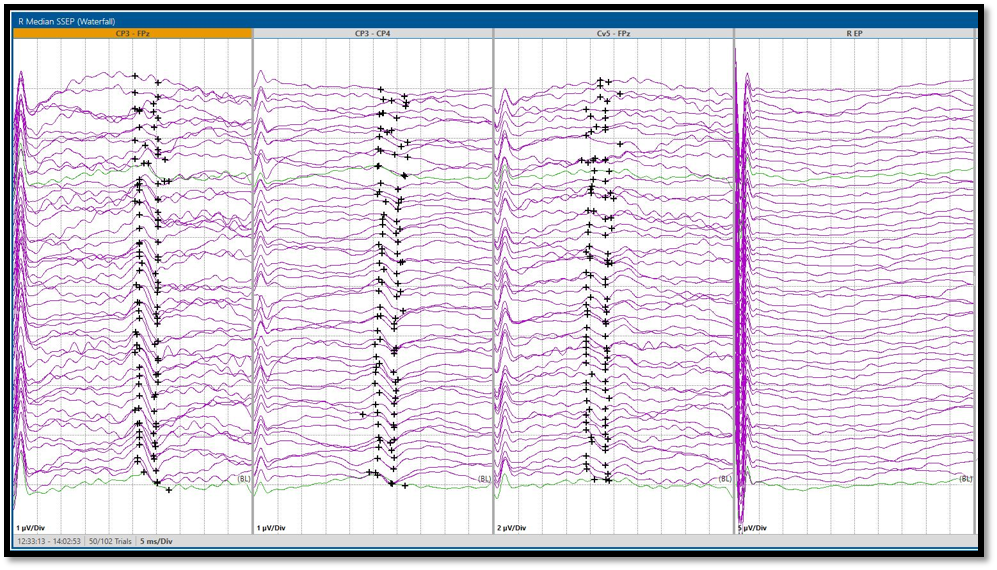
Figure 3: Right C6 Dermatomal SSEP (Median nerve) responses in a stack with absent baseline (Red arrow) and reproducible closing responses (Blue arrow).
Discussion:
The median nerve passes through the carpal tunnel along with tendons of hand muscles under the flexor retinaculum and enters the hand. It divides into the digital cutaneous sensory branch, and recurrent muscular branch. The recurrent muscular branch of the median nerve supplies the first and second lumbrical muscles and the thenar muscles (opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis). The ulnar nerve innervates the remaining intrinsic muscles and adductor pollicis brevis muscle. The median nerve innervates the skin of the palmar surface of the hand, thumb, index finger, and the middle finger. The palmar cutaneous branch of the median nerve supplies the radial aspect of the hand.
Hand injuries can result in damage to the motor and sensory branches of the median nerve. Damage to the sensory branches can result in loss of the sensory function of the palmar surface of the hand and sensations to the thumb and first two fingers. Any injury to the motor branch may result in the loss of motor function of the hand.
Utilizing the multimodality IONM with SSEP, TCeMEP, s-EMG, and t-EMG during peripheral nerve surgeries can be highly beneficial to the patient and as well as the surgeon. Real-time feedback to the surgeon about the nerves can help the surgeon to make the best decision, which may alter the course of treatment. IONM can also minimize any postoperative neurological deficits involving the motor function.
Conclusion:
In this patient, a multimodality IONM was used effectively for the evaluation of the neural function intra-operatively. The neurophysiological monitoring utilizing DSEP and EMG helped in directing the surgeon intra-operatively. During surgeries that put the peripheral nerves at risk of injury, continuous
monitoring of the function is desirable.
The intraoperative neuromonitoring was performed by a CNIM certified technologist and a D.ABNM board-certified neurophysiologist. A board-certified neurologist with a specialty in IONM was also present online for remote monitoring during the entire surgical procedure.
Results:
In this patient, the IONM helped in guiding the surgeon during the high-risk procedure. Due to improved DSEP and TCeMEP responses, the surgeon decided to changed the course of treatment to minimize any postoperative neurological deficit and better patient outcome.
References:
[1] Jahangiri FR. Multimodality neurophysiological monitoring during tibial/fibular osteotomies for preventing peripheral nerve injuries. Neurodiagn J. 2013;53(2):153?168.
[2] Happel L.T., Kline D.G. (2017) Surgery in the Peripheral Nervous System. In: Koht A., Sloan T., Toleikis J. (eds) Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals. Springer, Cham.
[3] Happel L, Kline D. Intraoperative neurophysiology of the peripheral nervous system. In: Deletis V, Shils J, editors. Neurophysiology in neurosurgery. New York: Academic; 2002. p. 169–94.
[4] Jahangiri FR, Blaylock J, Qadir N, Ramsey JA. Multimodality Intraoperative Neurophysiological Monitoring (IONM) During Shoulder Surgeries. Neurodiagn J. 2020;1?17. doi:10.1080/21646821.2020.1743952.
[5] Jahangiri FR, Qadir N, Blaylock J, Cronce-Solano L, Ramsey J. Waveform Window #46: Radial Nerve SSEP (Rn-SSEP): Is It Reliable?. Neurodiagn J. 2019;59(4):232?235. doi:10.1080/21646821.2019.1680085.
[6] Jahangiri, FR. Surgical Neurophysiology: An Introduction to Intraoperative Neurophysiological Monitoring (IONM). Second Edition. April 2012.
[7] Kline DG, Happel LT. Penfield Lecture. A quarter century's experience with intraoperative nerve action potential recording. Can J Neurol Sci. 1993;20(1):3?10. doi:10.1017/s0317167100047338
[8] ABRET Neurodiagnostic Credentialing and Accreditation. (2019, Sep 9). ABRET. Retrieved Sep 9, 2019, from ABRET: https://www.abret.org/candidates/credentials/cnim/
[9] ABNM: American Board of Neurophysiologic Monitoring. (2019, Sep 9). ABNM: American Board of Neurophysiologic Monitoring. Retrieved Sep 9, 2019, from ABNM: American Board of Neurophysiologic Monitoring: http://www.abnm.info/
[10] Gertsch JH, Moreira JJ, Lee GR, Hastings JD, Ritzl E, Eccher MA, Cohen BA, Shils JL, McCaffrey MT, Balzer GK, Balzer JR, Boucharel W, Guo L, Hanson LL, Hemmer LB, Jahangiri FR, Mendez Vigil JA, Vogel RW, Wierzbowski LR, Wilent WB, Zuccaro JS, Yingling CD; membership of the ASNM. (2019). Practice guidelines for the supervising professional: intraoperative neurophysiological monitoring. J Clin Monit Comput, 33(2), 175-183. doi:10.1007/s10877-018-0201-9



